Cardiology Case #13
Primary Author: Dr Alastair Robertson; Co-Authors: Dr Hywel James and David Law
Background:
A 45 year old male presents to ED overnight having woken 30minutes ago with central chest discomfort and breathlessness.
He is a non-smoker with no significant past medical history.
His observations are: RR 25, Sats 98% on air, HR 110, BP 160/90, temp 36.5, GCS 15.
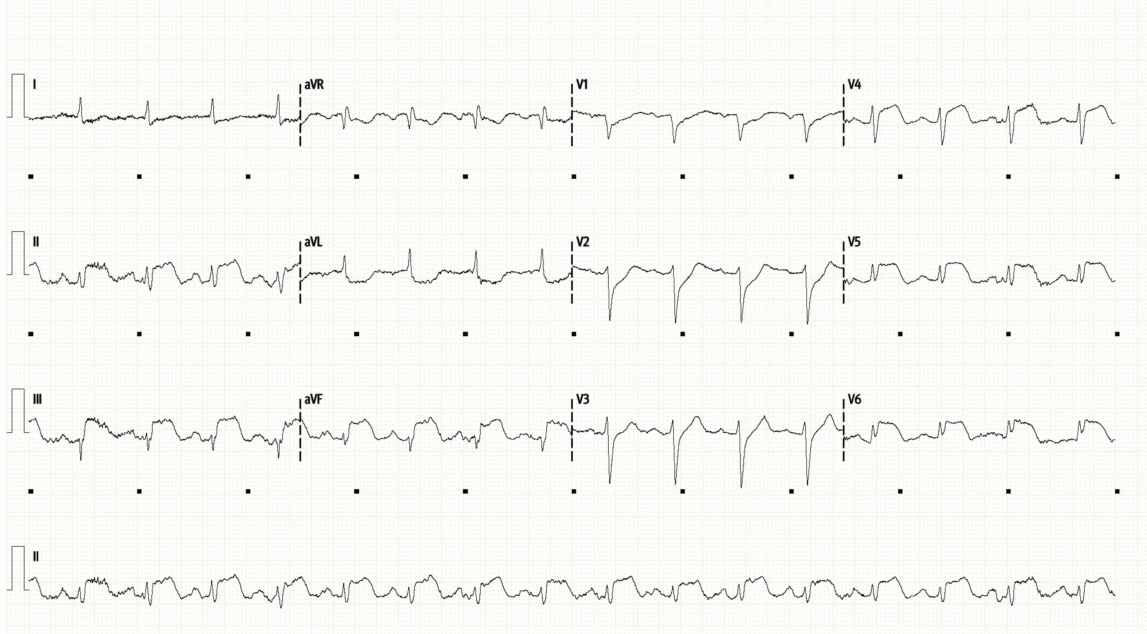
His ECG is below, what are your differentials?
-
This is a concerning ECG. Rhythm is sinus with a rate of around 95/min.
There is ST elevation and hyper-acute T-waves in the infero-lateral leads (II, III, aVF, V5, V6).
There is reciprocal ST depression in leads I and aVL. There is also ST depression anteriorly (V1, V2) suggesting posterior involvement.
There is left-axis deviation and poor R-wave progression in precordial leads.
This is an infero-postero-lateral STEMI.
Are there any differentials other than myocardial ischaemia?
In this context, chest pain associated inferior changes, tachycardia, and hypertension, should prompt consideration of acute aortic dissection. POCUS can be useful in rapidly assessing for this as a differential, although gold-standard imaging is a CT aortogram.
Features that may be associated with acute dissection include:
Pain character: sudden onset, tearing, radiating to back
Clinical features such as pulse defecit, limb ischaemic, acute neurology
Risk factors e.g. connective tissue disease, prior aortic surgery, aortitis.
Widened mediastinum on CXR (or other CXR findings)
Echo features including:
Pericardial effusion and/or tamponade
Acute Aortic Valve Regurgitation
Aortic root dilation (dissection flap can be seen on PLAX in aortic root, or in descending aorta)
Aortic arch dilation, or dissection flap in arch with parallel flows on colour doppler.
Regional wall motion abnormality due to dissection into coronary arteries (most commonly the RCA as just above the right sinus of valsalva is the most common start point for acute dissection).
Case Progress:
Chest XR (shown above) did not show mediastinal widening and lung fields were clear.
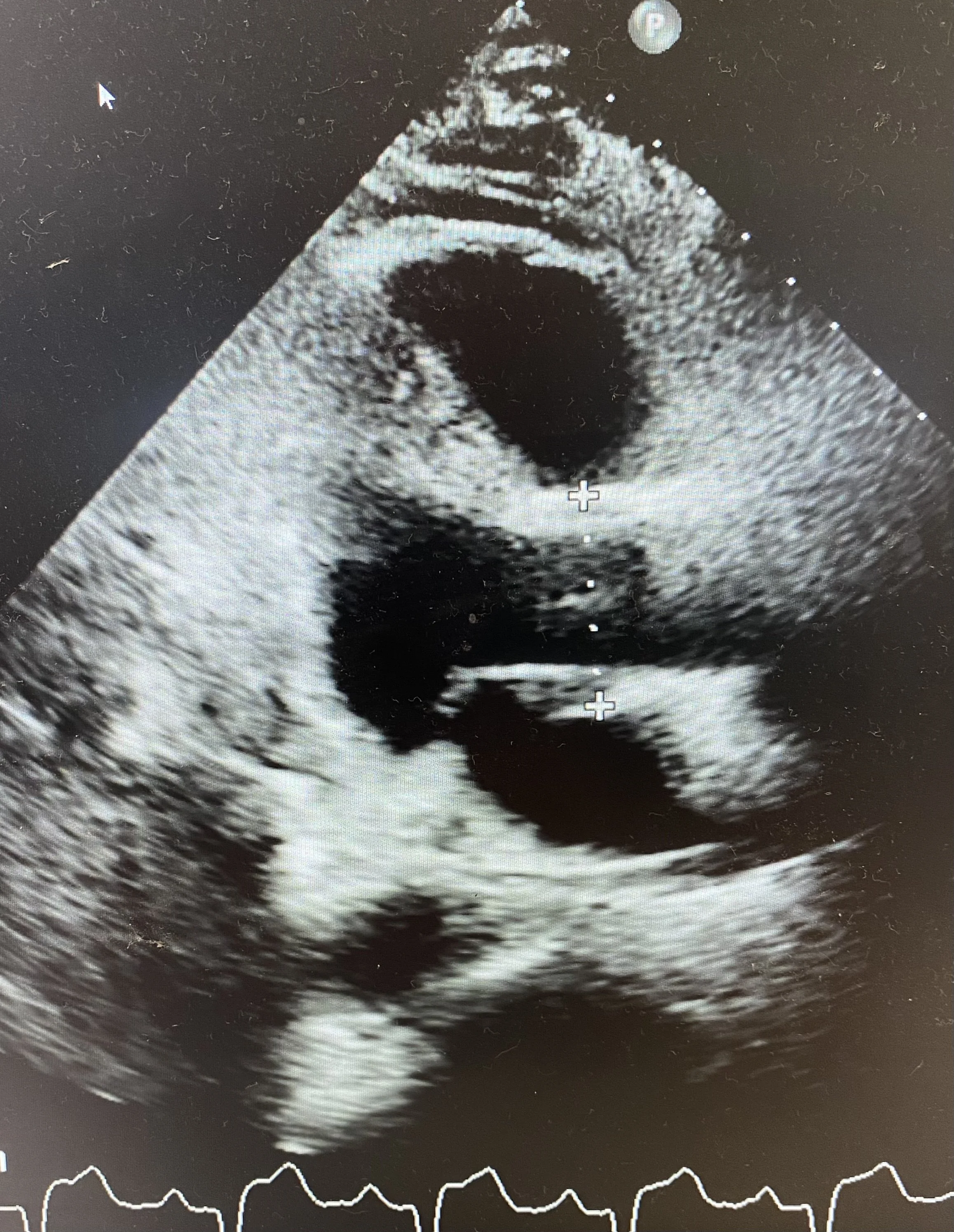
POCUS (shown below) showed a normal size aortic root and ascending aorta. There was no pericardial effusion.
There were no other features suggestive of acute aortic dissection making Occlusion MI the most likely diagnosis.
See stills showing measurement of the Aortic Root (top) and the Ascending Aorta (bottom). From the Parasternal long-axis you may need to rotate the probe to open up the aortic root and measure the maximum width. Ensure the ascending aorta is measured above the sinutubular junction. Sometimes moving the probe up a whole rib-space allows the ascending aorta to be better visualised.
The measurements here were 3.8cm and 3.5cm respectively for aortic root and ascending aorta (normal).
Basic POCUS:
This case has been included as the echo beautifully shows regional wall motion abnormality in keeping with the suspected pathology from the ECG.
Review the diagram below to remind yourself of the LV territories in different apical views, and the short-axis views.
The top clip is a parasternal long-axis. Note how the anterior septum (LAD territory) is contracting in whereas the posterior wall is hypo kinetic and not contracting (appears to just be ‘rocking’). The posterior wall is generally RCA or LCx territory.
The PLAX also shows a trivial pericardial effusion, good opening of mitral and aortic valves, and a normal appearing RV.
The bottom clip is a parasternal short axis. The anterior part of the LV is contracting well (Anterior Septum 10-12 o’clock, and Anterior Free Wall 12-2 o’clock). These are supplied by the LAD. The inferior and posterior walls are not contracting inwards. There is also poor contractility in the lateral wall (2 to 4 o’clock). This is consistent with inferior, posterior, and lateral infarction. Given lateral involvement on echo and ECG a LCx lesion was suspected.
Intermediate POCUS:
Assessing for complications of MI
Mitral regurgitation is a common complication of Inferior MIs due the impact on the poster-medial papillary muscle. It is important to assess for significant MR as this requires careful haemodynamic management.
Note the MR jet in this parasternal long-axis image. The MR is only mild as the jet is narrow, and does not wrap around the wall of the atrium (so called ‘eccentric jets’). If the MR was severe, you would expect a large and/or eccentric MR jet, as well as a hyper-dynamic LV and evidence of raised pulmonary pressures/pulmonary oedema.
Use of Apical Views
Use of the apical views is important to visualise the key vascular territories. Below is an Apical Long-axis (also called Apical 3-Chamber). This shows the same LV walls as a PLAX, but visualises the apex far better, allowing exclusion of apical hyperkinesis, as well as complications such as apical thrombus. Note the marked hypokinesis on the posterior wall (left of screen) compared to the anterior septum (right of screen).
FOCUS on Inferior MI
A quick re-cap on Inferior MI
Assess for posterior and lateral involvement as well.
Assess for Mitral Regurgitation, which can occur due to papillary muscle dysfunction, or even rupture (this will cause catastrophic MR).
Inferior STEMI can be due to occlusion of: the
RCA (around 80% of cases)
LCx (around 18% of cases) - see Case #11
Wraparound LAD (around 2% of cases) - see Case #6
Case Conclusion
The patient was thrombolysed with Tenecteplase as Primary PCI was not available. His pain improved but ST elevation on his ECG initially worsened (top ECG), before finally resolving at 1 hour post-thrombolysis (bottom ECG).
ECG at 10 minutes post-thrombolysis (above). Note the worsening ST elevation in both inferior and lateral leads. He remained haemodynamically stable and the ECG below shows that ST segments have largely normalised by 60 minutes post-thrombolysis.
The patient subsequently developed a recurrence of chest pain on CCU which was refractory to GTN and was taken for Rescue PCI. He had an LCx lesion (see below - centre of clip) which was stented with good results.