Cardiology Case #12
Primary Author: Dr Alastair Robertson; Co-Authors: Dr Hywel James and David Law
Background:
A 53 year old man presented to ED with 1 week of cough and exertional breathlessness.
Initial observations were RR 20, Sats 94% on 2L O2, HR 106, BP 118/74, temp 36.7.
Physical examination was unremarkable.
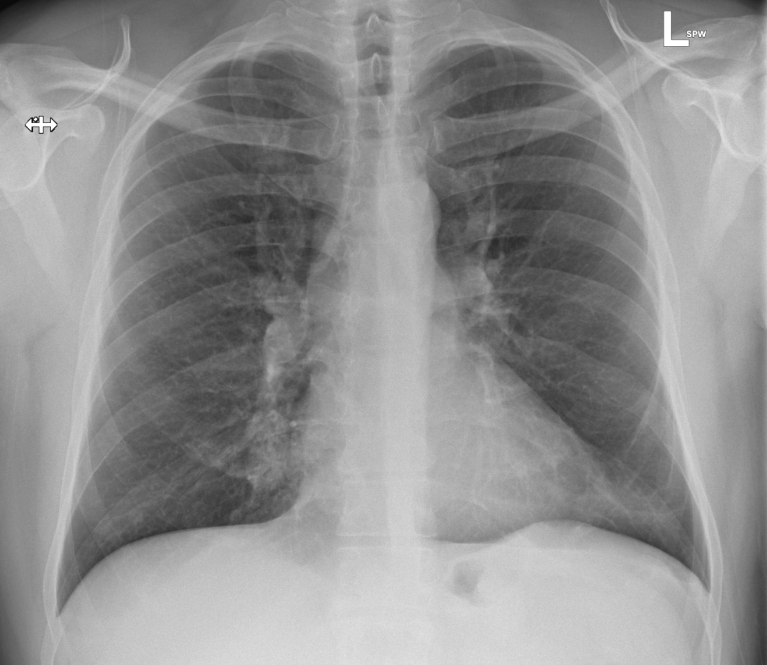
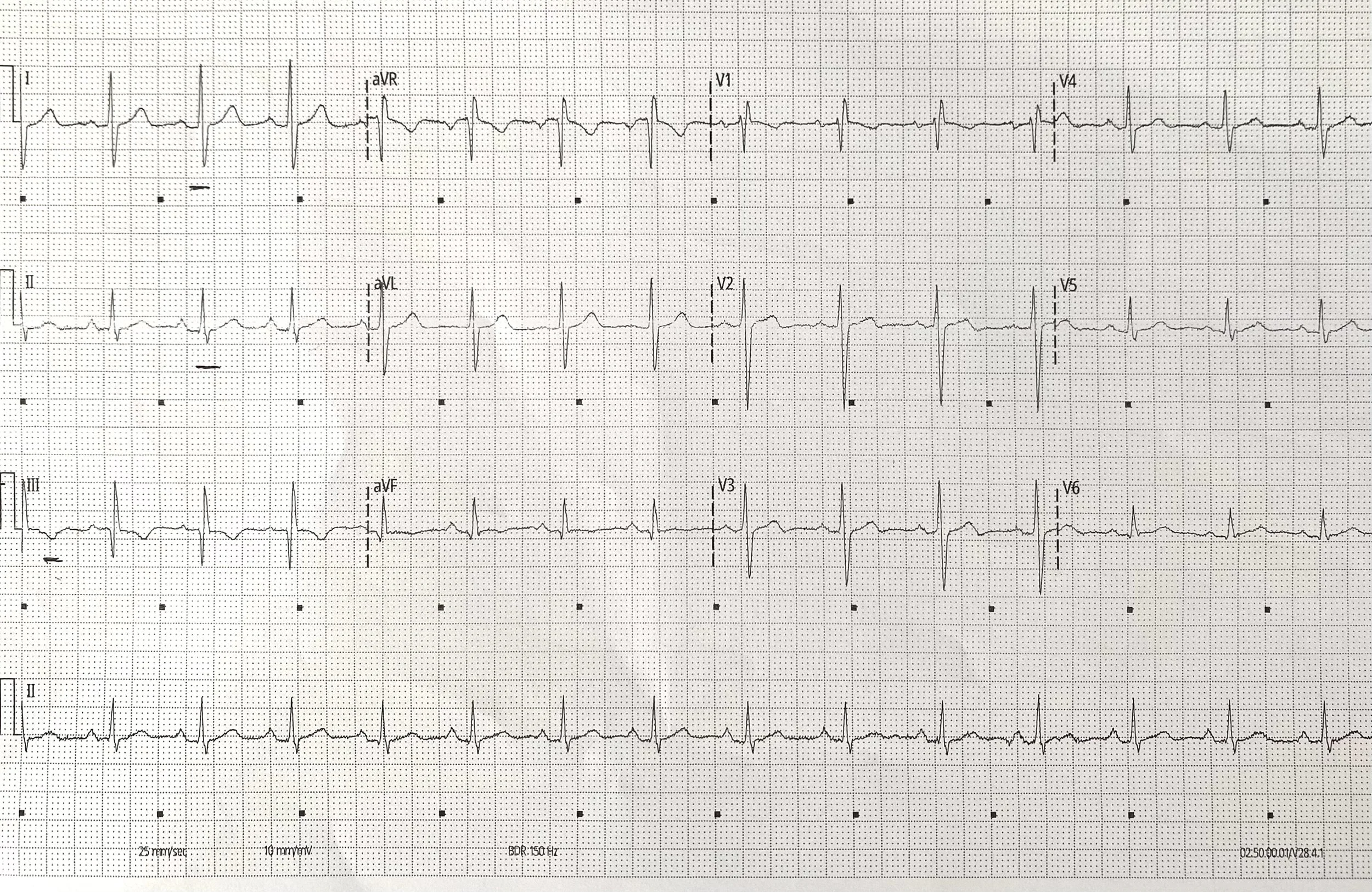
His CXR and ECG are shown below, what do you think?
-
Lung fields are largely clear, there is no pneumothorax, pulmonary oedema, or cardiomegaly visible.
Patchy pacifications at the right mid-zone (with loss of right heart border) and left lower zones raise possibility of infection. They could also however represent e.g. pulmonary infarction.
-
Sinus rhythm at 90/min. No significant ST changes or evidence of RV strain.. There is a R wave in aVR. There is also RAD with an S1Q3T3 pattern (which whilst a ‘classic’ finding for PE, is neither particularly sensitive or specific.
What is your differential?
Cardiac POCUS:
In this case cardiac POCUS was used to assess the heart, looking for features which would explain his presentation including pericardial effusion, cardiomyopathy, pulmonary embolism, valvular pathology.
What do you think is going on?
∞ SPACE REPETITION
Work through the images below by ASKING yourself….
- is there a pericardial effusion? AND if so, signs of tamponade?
- is there signs of Right heart strain (1:1:1) rule
- is there LV impairment?
- is there signs of hypovolaemia?
-
Video 1 is a parasternal long-axis. There is no pericardial effusion. the RV may appear mildly dilated. The LV is not dilated and has good systolic function. Aortic and mitral valves are opening well and look grossly normal.
Video 2 is a parasternal short-axis. The LV should be circular, but the septum is being compressed inwards by the RV. This is a D-shaped septum suggestive of raised pulmonary pressures.
Video 3 is an apical 4-chamber view. The RV looks dilated (it appears larger than the LV), and has poor function, with the exception of the RV apex which appears hyper-dynamic. This is McConnell’s sign.
These features are all suggestive of acute PE.
Case Progress:
Pulmonary embolus was highly suspected and subsequently confirmed with CTPA.
The patient remained haemodynamically stable.
Image below shows an axial slice of CTPA showing bilateral PEs
Basic POCUS - Pulmonary Embolism:
Assessing for RV strain
2D Echo utilising basic echo views can be a crucial tool in demonstrating evidence of RV strain secondary to PE.
Features include:
Dilated/enlarged RV on PLAX
The RV or RVOT should be approximately the same size as the aortic root, and the left atrium on the parasternal long-axis. This 1:1:1 rule can be a first step in assessing for a dilated RV, aortic root, or left atrium. In video 1 above the RV appears only mildly dilated.
D-shaped Septum on PSAX
From parasternal long-axis, rotate the probe 90 degrees clockwise (marker now pointing 1-2 o’clock or towards patient’s left shoulder). The LV should be visible as a circular structure. Aim to visualise the LV base (there should be ‘broken lines’ of the chordae in view, if you see the ‘fish-mouth’ mitral valve fan toward the apex slighly). The interventricular septum sits from around 8-12 o’clock. If right ventricle pressures are high the septum bows into the left ventricle, giving a D-shape rather than a round shape as seen in the video 2 above.
Enlarged RV on A4C
Assessing RV size is best done from apical views, but can be difficult. The RV size should generally be around two thirds of the LV size. It is however easy to create the appearance of a dilated RV by cutting through the RV obliquely with a view that is too medial (probe position antero-medially). To get an ‘RV focussed view’ ensure you have hooked the probe laterally from a classical 4-chamber view which will give you the true RV size. See video 3 above.
McConnell’s Sign on A4C
In acute PE with associated RV strain, the RV systolic function is impaired. The classic pattern is of hypokinesis of the RV free wall (the left RV border on the video above) whist the RV apex has preserved, or even hyper-dynamic function. Look above to see how the apex is working well, but the free wall is hypokinetic. It is sometimes described as imagining a tiny man jumping on a trampoline on the RV apex.
Intermediate POCUS - Pulmonary Embolism:
Further assessment of PE and haemodynamic compromise
Further echo techniques are particularly useful in assessing for evidence of PE causing haemodynamic compromise. Especially given how tricky it can sometimes be to get good 2D imaging of the RV
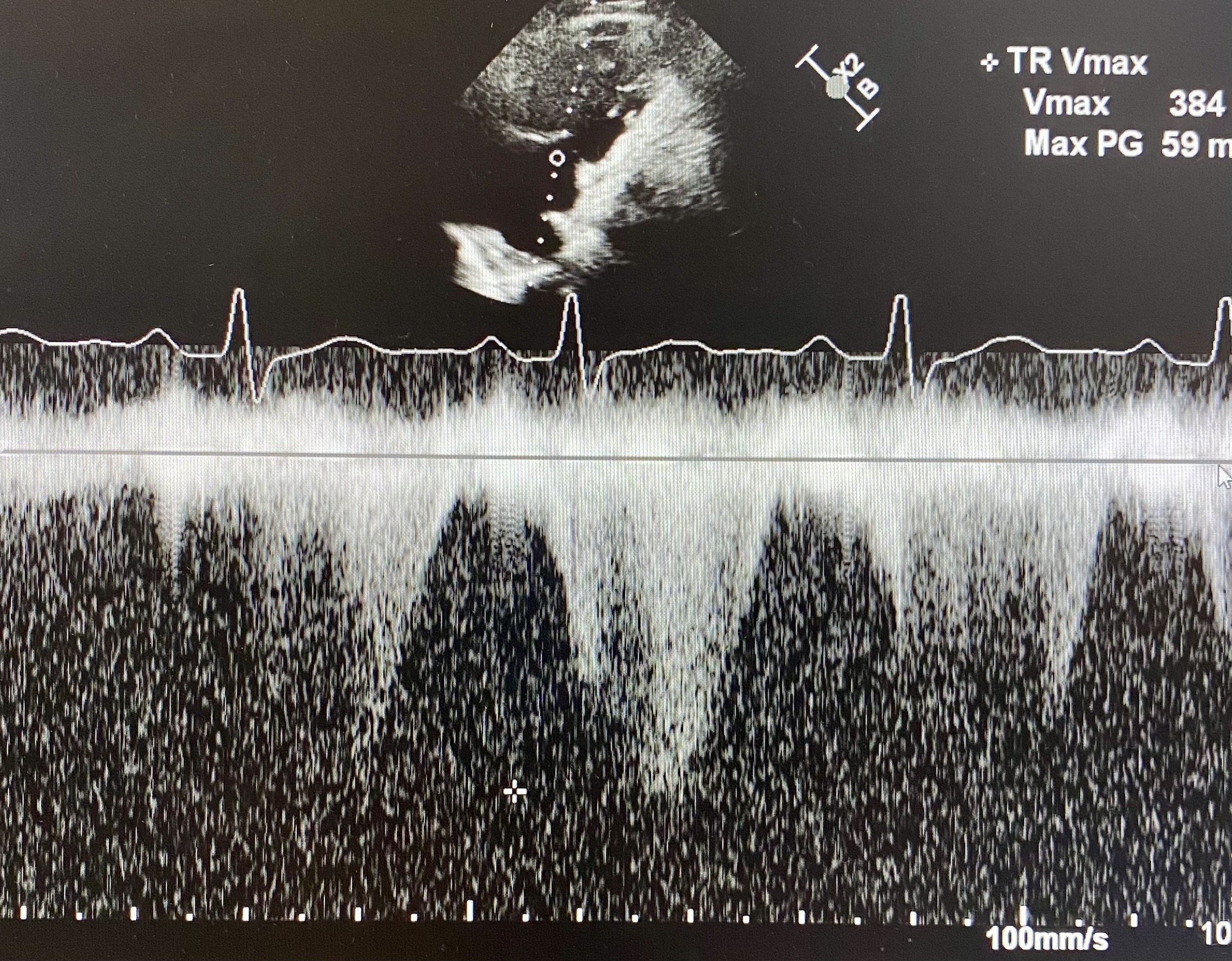
1) Measuring Pulmonary Pressures
Quantifying pulmonary pressures with the use of doppler is key to many right-heart pathologies. Measuring PASP (Pulmonary Artery Systolic Pressure) is a two-step process.
i) Measure RVSP (RV Systolic Pressure) which is the pressure difference between the RV and the right atrium. To calculate this identify the tricuspid regurgitation jet using colour doppler. This is usually done from an Apical 4-Chamber view. Here you can move the probe medially can get a better TR jet (although it will obliquely cut the RV making it looking larger than it is in 2D). Once the TR jet is identified put CW Doppler through the jet. A good doppler signal will be a symmetrical parabola (see below). The apex of the parabola is the TR Vmax, and the US machine can use this to calculate the RVSP in mmHg (equation is RVSP = 4 x (TR Vmax)^2)
ii) To calculate the PASP you need to add the RAP (Right atrial pressure) onto the RVSP. This is estimated from the IVC:
RAP = 12mmHg if IVC >2cm and <50% collapse with respiration
RAP = 8mmHg if IVC >2cm but >50% collapse or IVC <2cm and <50% collapse
RAP = 5mmHg if IVC <2cm and >50% collapse
Adding RAP to RVSP will get an estimate PASP. PASP >40mmHg is elevated.
Gold-standard measurement of pulmonary pressures is via right-heart catheterisation.
Remember there are many causes of pulmonary hypertension including:
Pulmonary artery HTN (inherited/idiopathic, sympathomimetics, neonatal PPHN)
Left heart disease (valve disease, shunts, congenital lesions)
Lung disease (COPD, interstitial lung disease, OSA, chronic altitude)
VTE (e.g. pulmonary embolism or rarer causes e.g. vasculitis)
Multi-factorial
In this patient assessment of the TR jet showed RVSP of 59mmHg (see cross and automatic calculation by machine) which is severely elevated. The RAP was estimated to be around 8 giving a PASP of 67mmHg.
This is severely elevated pulmonary pressures supporting the diagnosis of acute PE with significant obstructive effects on the right heart.
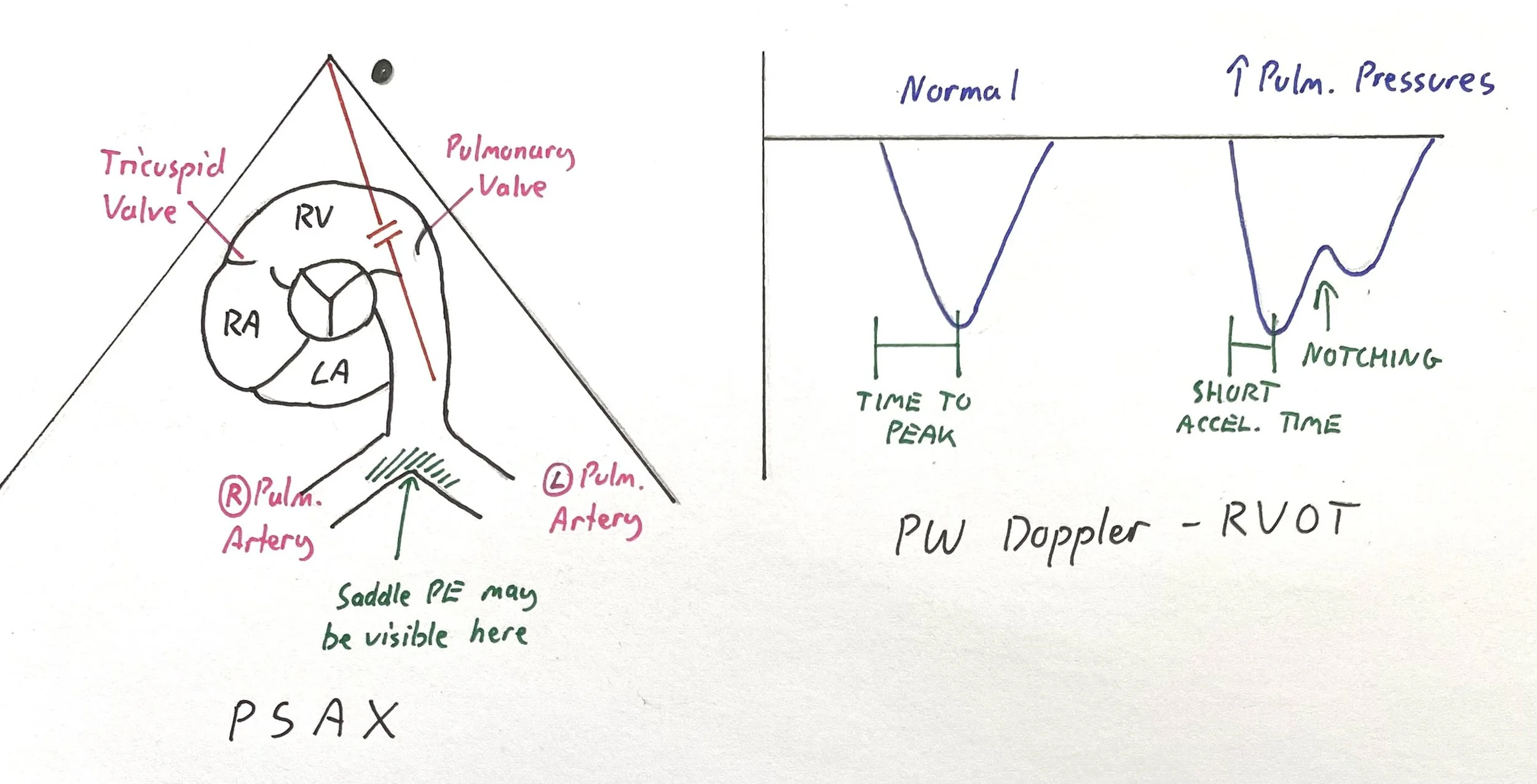
2) Intermediate/Advance POCUS: Assessing the Right Ventricular Outflow Tract
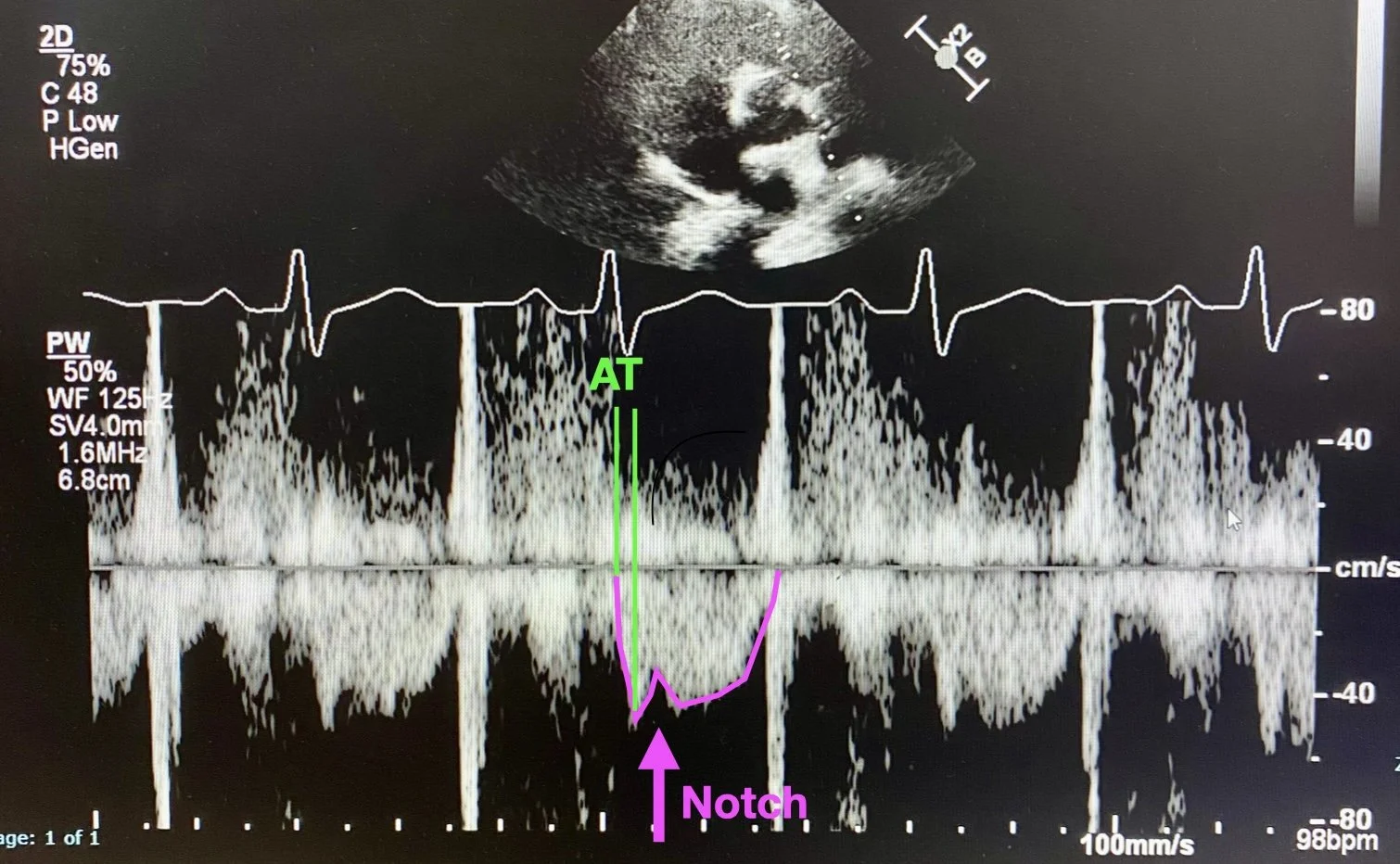
The use of doppler signal can detect RV outflow in the RVOT and pulmonary trunk. Obtain a parasternal short axis, at the level of the aortic valve. The RV wraps around the top of the valve with the pulmonary valve typically sitting at 2-3 o’clock to the aortic valve (see diagram below). By placing PW doppler in the RVOT (just before the pulmonary valve) you will get the RVOT tracing.
A normal RVOT trace is triangular, and the Acceleration Time (time from start to peak) should be >100ms (assuming a relatively normal HR). In acute PE you see features of raised pulmonary pressures which include:
Notching of the RVOT doppler trace
Short acceleration time (often around 60ms in acute PE)
In the left hand diagram (PSAX view) you can see the right heart ‘wrapping around’ the aortic valve in the centre. Place PW Doppler just before the pulmonary valve.
The right hand diagram shows the PW doppler traces you would see with normal pulmonary pressures (left) and in raised pulmonary pressures (right) including notching and a short acceleration time. Both of these suggest elevated pulmonary pressures, notching in particular is very specific. Acute PE with right heart strain should cause raised pulmonary pressures.
This is the RVOT PW Doppler tracing from this patient. Note the trace (outlined in pink) with dramatic notching (pink arrow). Also note the Acceleration Time - in this case it measured at 40ms which is incredibly short.
Both of these features indicated elevated pulmonary pressures, which in this case was consistent with Acute PE and associated right heart strain.
3) Visualise the Pulmonary Trunk
A final useful skill is to visualise the pulmonary trunk directly to assess for saddle PE sitting at the bifurcation.
Review the diagram above so see where the Pulmonary Trunk bifurcation sits in relation to the aortic valve in the PSAX view.
The video below shows a fantastic view of the pulmonary trunk bifurcation into left and right pulmonary arteries which does not show a saddle embolism. CTPA also confirmed there was no saddle PE, but large-burden left and right sided PEs.
FOCUS on PE
Above are some key tips for visualising signs of RV strain associated with acute PE using both 2D echo, and Doppler echo.
The important question is always:
Is This Patient in Obstructive Shock?
Massive PE is defined as PE with cardiac arrest, hypotension (BP <90 or drop of >40 from usual for 15mins), persistent bradycardia, or requirement for vasoactive medications.
Sub-massive PE is less well defined, but generally considered be evidence of RV strain, or early shock/haemodynamic compromise and management of these patients lacks clear evidence.
One way to assess for early haemodynamic compromise is to measure the Stroke Volume using PW doppler in the LVOT (see Case #10). Excluding shunts or regurgitant valves, the RV stroke volume should = the LV stroke volume.
If the stroke volume and/or cardiac output is decreased, this indicates an obstructive shock state.
Case Conclusion:
The patient was admitted for ICU for close monitoring and anticoagulation. He did well, and did not require thrombolysis. He was discharged from hospital on a DOAC.
Crashing PE Management
As an aside let’s quickly review an approach to management of the crashing or peri-arrest PE patient in ED.
Thrombolysis for Massive PE - usually at “full-dose”
Alteplase 100mg (10mg bolus, rest over 2 hours), or
Tenecteplase 0.5mg/kg as a push
In cardiac arrest use Alteplase or Tenecteplase as a 50mg push.
Support oxygenation
100% O2, consider NIV, avoid intubation if at all possible
Optimise pulmonary vasodilation
consider nebulised GTN or milrinone
consider iNO or inhaled/IV prostacyclin as pulmonary vasodilators
Avoid pulmonary vasoconstriction/RV failure by avoiding:
PEEP, hypercapnoea, acidosis, or excessive fluid load
Support haemodynamics
no good evidence for any one particular vasopressor
Adrenaline a reasonable first-line inopressor
Consider adding vasopressin (relative sparing of pulmonary vasculature)
Referral for VA ECMO if available
In cardiac arrest consider prolonged CPR to allow thrombolysis to work.