Cardiology Case #7
Primary Author: Dr Alastair Robertson; Co-Authors: Dr Hywel James and David Law
Background:
A 70 year-old gentleman presents to ED with significant new-onset breathlessness on exertion over the last week. He describes some central chest heaviness and orthopnoea.
He is otherwise well, usually fit and active, and has no other past medical history.
Examination revealed a systolic murmur
ECG and CXR are shown below.
-
ECG shows multifocal ventricular bigeminy with an absolute rate of 90bpm. The ventricular beats come from alternate foci. There is left axis deviation but no significant ST changes and (importantly with frequent PVCs), a QTc of 490ms.
Chest XR shows a markedly enlarged cardiac silhouette with clear lung fields. Subtle blunting of the left costophrenic angle, and possibly a left apical opacification.
Cardiac POCUS
Parasternal Long axis views
-
The parasternal long-axis gives a lot of information about the heart here.
The LV is dilated, but is contracting well, with an high/normal EF (hyper -dynamic appearance).
The mitral valve looks abnormal and the top (anterior) leaflet is bowing back into the left atrium - this immediately raises concern for significant mitral regurgitation.
The left atrium appears dilated, which would be consistent with MR.
The RV and aortic root appear normal, the aortic valve is opening well (excluding severe AS), and there is no significant pericardial effusion.
Putting colour over the mitral valve shows a large regurgitant jet filling the entire of the LA. This is severe MR.
Given the clinical presentation a diagnosis of acute severe mitral regurgitation was made. Further views were obtained to ascertain the cause, as well as the severity.
POCUS Pearls:
Stepping into valve assessment
A good parasternal view is key to getting an idea of how the heart is functioning. In the video below close inspection of the mitral valve using the zoom function showed a prolapsing mitral valve. The colour doppler above shows that this is severe mitral regurgitation.
To get colour, position the colour box near the bottom of the screen, and size it to cover the entire left atrium so as to not miss eccentric MR jets which may track round the posterior wall.
Intermediate POCUS:
In the below clips, the apical 4-chamber view shows the dilated LV and flail mitral valve. Colour doppler shows the severe MR wrapping all the way round the left atrium.
Extra Tips: Intermediate skills
Elevated pulmonary pressures are a complication of acute mitral regurgitation.
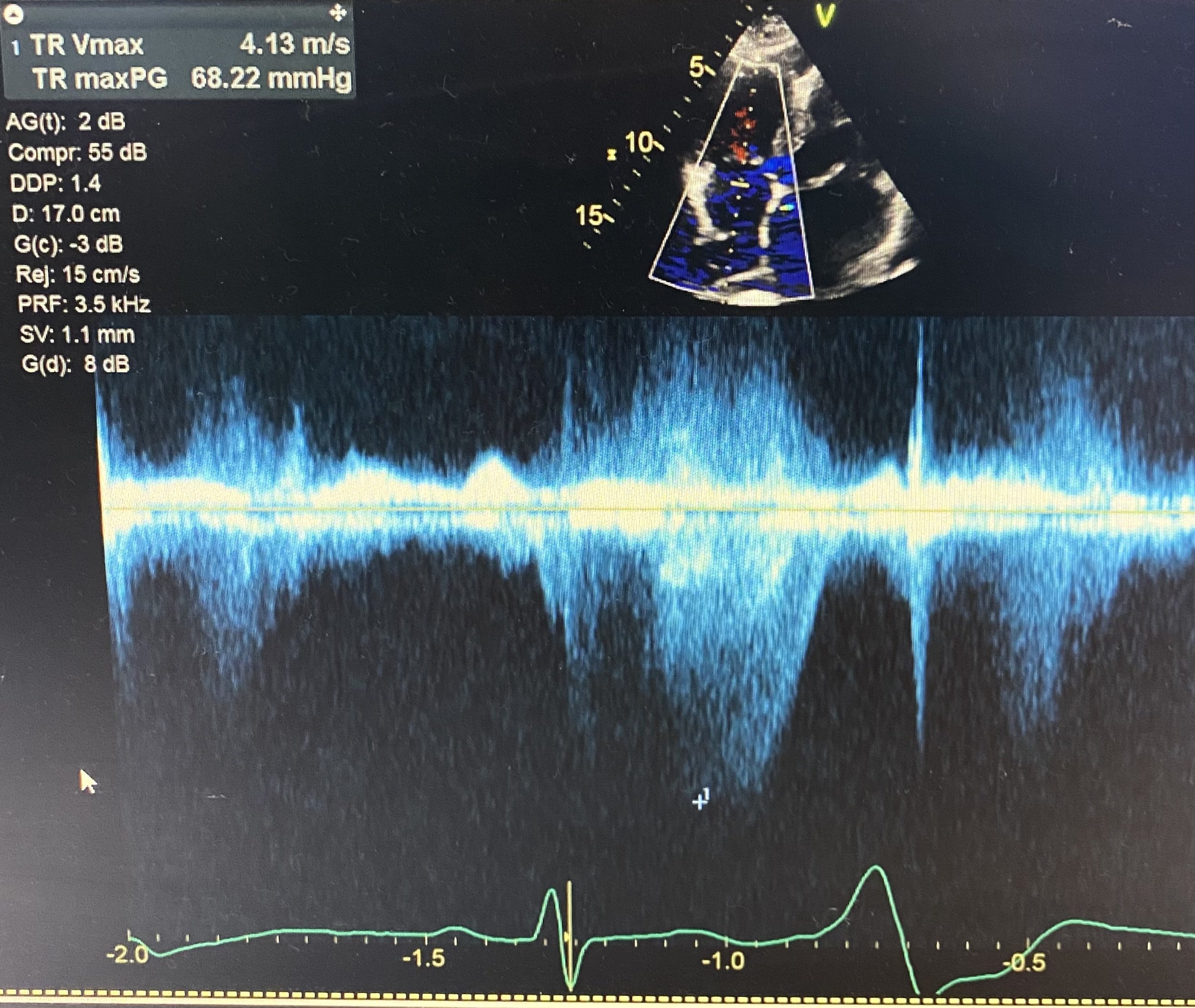
By locating the TR jet in a 4-chamber view and then putting CW doppler through the TR you can calculate the TR Vmax and thus the RV systolic pressure (RVSP).
Our patient has severely elevated pressures. RVSP is 68mmHg and the right atrial pressure (measured from IVC diameter/collapsability) will be an additional 12-18mmHg. (Normal systolic pulmonary pressures are below 40mmHg).
Case Conclusion
This patient had acute mitral regurgitation secondary to a spontaneous chordae tendinae rupture. He developed pulmonary oedema as well as new Atrial Fibrillation with RVR whilst being monitored in CCU.
His AF was controlled with amiodarone, he was diuresed, and fortunately remained haemodynamically stable. He was transferred urgently for surgical intervention to repair his flail valve.
FOCUS on Acute Mitral Regurgitation
Acute Severe Mitral Regurgitation is a valvular catastrophe that must be managed well in ED.
The common causes are:
Intrinsic Valvular: Endocarditis, Papillary Muscle rupture (classically from infero-posterior MI), chest trauma, chordae rupture (myxomatous, rheumatic, spontaneous), leaflet perforation, congenital abnormalities.
Non-valvular: Dynamic LVOTO, LV dilation (e.g. cardiomyopathy)
Classic Features: include
increased pulmonary pressures and pulmonary oedema
Hyper-dynamic LV on echo with tacyhcardia
On echo: large MR jet (>40% LA area) or eccentric jet (typically wrapping around the anterior or posterior wall)
Arrhythmia e.g. AF due to LA dilation
Management: involves addressing the complications:
These are volume-dependent lesions
Target lowest acceptable BP - consider afterload reduction if haemodynamics will allow. If in frank cardiogenic shock patients will require concurrent inotropy.
Expect a hyperdynamic LV and tachycardia - this is a compensatory response to maintain cardiac output
Manage pulmonary hypertension - NIV for pulmonary oedema, optimise oxygenation to avoid pulmonary vasoconstriction, if evidence of RV failure then ensure adequate preload and maintain blood pressure to ensure RV perfusion at higher RV pressures.
Address arrhythmia - AF is common and is often not tolerated well. Consider treating aggressively. Avoid beta-blockade where possible (due to negative inotropy).
Consider mechanical supports as a bridge to definitive therapy (e.g. ECMO, balloon pump)
Early surgical consultation for definitive management.