Cardiology Case #8
Primary Author: Dr Alastair Robertson; Co-Authors: Dr Hywel James and David Law
Background:
An otherwise well 18 year old football player presented with palpitations. They were noted to be in a sinus rhythm on the monitor, with runs of tachyarrythmia. There was no concerning family history.
Their ECGs are shown below, what do you think?
ECG 1
ECG 2
-
ECG 1: sinus arrhythmia with a rate of 48. BER and borderline LVH by voltage criteria. Intervals (PR, QRS, QT) are normal.
ECG2: regular narrow complex tachycardia with a rate of 120/min. QRS morphology is unchanged. Biphasic T-waves in inferior leads were thought to likely represent retrograde P-waves. This was favoured to be a supraventricular tachycardia - in particular orthodromic AVRT - by the treating team in ED as the rate was thought probably too slow for atrial flutter.
Presentations such as this are not uncommon in paediatric or adolescent patients and it is possible they have an undiagnosed structural cardiac abnormality. In this case the differential considered included SVT (AVNRT vs AVRT), atrial flutter, WPW or even AF.
Case Progress:
The patient remained haemodynamically stable with self-limiting runs of tachyarrythmia with associated palpitations. Electrolytes were optimised and he was monitored overnight with episodes becoming less frequent.
POCUS Pearls:
POCUS can be useful as a rapid screening tool to exclude significant structural pathology prior to a formal TTE.
These echo views were all normal in this patient.
Below are some examples of important abnormalities that can be assessed and ruled in on echo.
POCUS echo assessment: normal and significant differentials
HOCM
Here a parasternal long-axis shows good LV function, the LV does not appear to be hypertrophied and there is no suggestion of LVOTO.
HOCM is typically characterised by significant hypertrophy of the LV (with wall thickness >15mm) and a small LV cavity. Can be assessed on parasternal short/long axis as well as A4C. There can also be systolic anterior motion (SAM) of the mitral valve causing LVOTO.
The clip below also shows a normal appearing RV and aortic valve, as well as no pericardial effusion (always consider myo-pericarditis and/or pericardial effusion when assessing younger patients with tachydysrythnias).
Aortic Valve:
Below you can see a parasternal short-axis view of the aortic valve, showing a normal tri-leaflet valve. Congenital bicuspid aortic valves can cause both stenosis and regurgitation.
Ebstein Anomaly
Here an apical 4-chamber view shows a normal appearing LV.
At the crux of the heart, the tricuspid valve inserts slightly closer to the apex than the mitral valve. In Ebstein anomaly this insertion is even closer to the apex (>7mm) with associated ‘atrialisation’ of part of the right ventricle.
If present, this abnormality can be seen in an A4C view and is associated with right atrial dilation.
Right Ventricle
Assessing the right ventricle with an ‘RV focussed’ A4C view is important. From an A4C view swing the probe laterally. This avoids artificially dilating the RV by eliminating an oblique cut through the RV.
If the RV appears normal, and the RV base is <4cm (see below) then significant L—>R shunt pathology is unlikely, as this would be expected to cause a dilated RV.
This is a still from an RV focussed view (note lateral swing compared to a ‘classic’ A4C) with measurement of the RV base, in this case 3.6cm (normal is <4cm).
Aortic Coarctation
Coarctation of the aorta is an important pathology to exclude, as this can be missed on prenatal scans and post-natal baby checks, and go undiagnosed until it causes significant complications.
The aorta can be identified from the subcostal view. Once you have identified the IVC in long axis (focus on the right atrium, then rotate the probe 90 degrees anticlockwise with marker pointing up towards the head), swing the probe slightly to the patient’s left. The aorta should be seen in long axis, running parallel to the IVC but usually slightly deeper.
It can also be identified using the curvilinear probe in the abdomen as you would when scanning for a AAA.
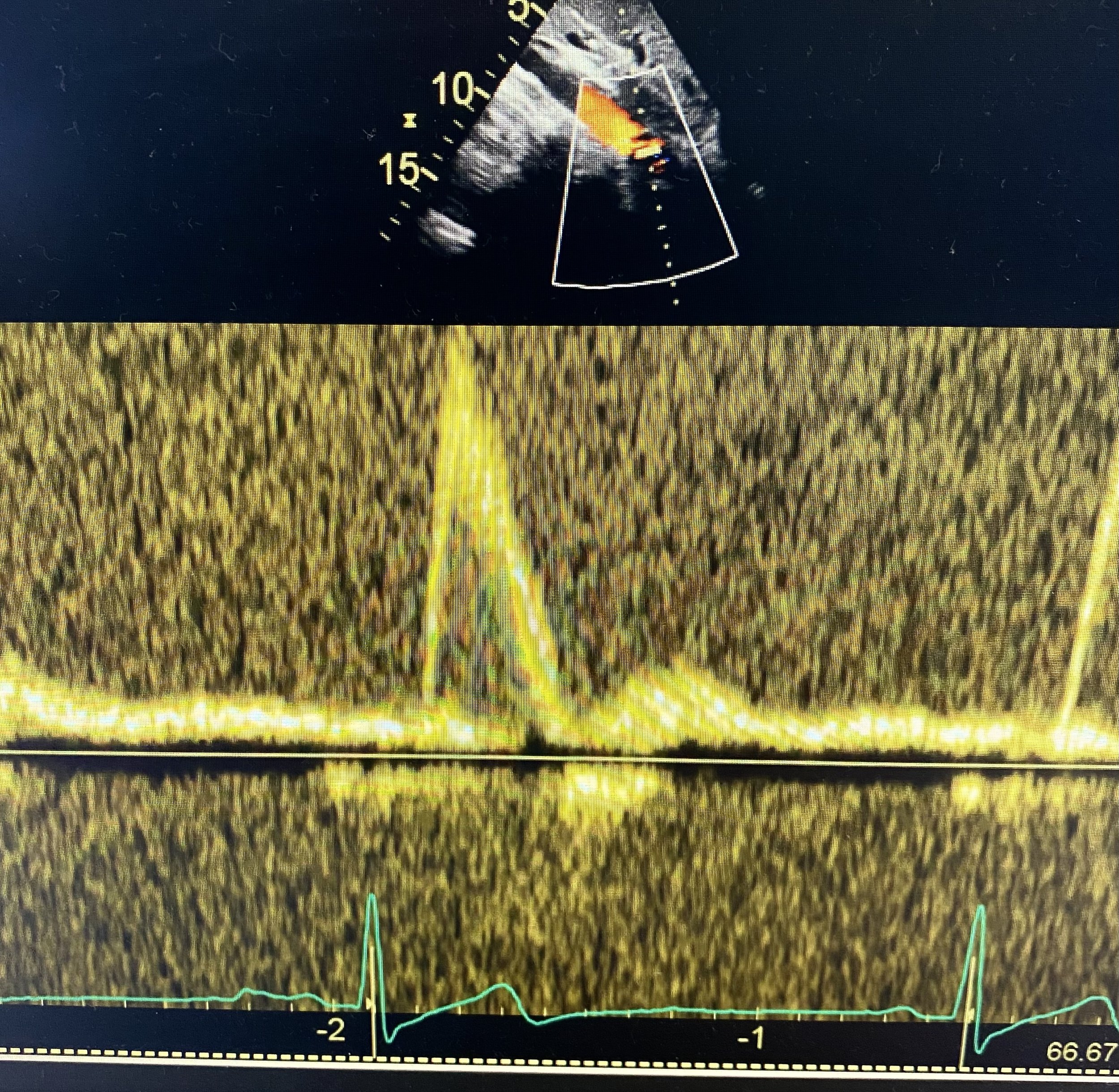
Once identified you can confirm with colour doppler to show pulsatile flow. Putting PW doppler onto the vessel to show a pulsatile waveform excludes a significant coarctation.
Video below shows colour doppler (top), then a still of PW doppler onto the vessel with pulsatile arterial flow (bottom).
Advanced POCUS
Other assessments in these patients may include:
Assess for ASD by putting colour doppler over the intra-atrial septum in the subcostal 4-chamber view. You will need to turn down the colour doppler velocity scale to see lower-velocity flows.
Assess for Pulmonary stenosis which can be missed as it is often minimally symptomatic. Put CW doppler through the pulmonary valve in the parasternal short-axis view when assessing the RV outflow tract. A pulmonary Vmax of <1.5m/s is normal.
Assess valves - careful visualisation of the valves to assess for congenital valvular abnormalities.
Case Conclusion
The patient was admitted on cardiac monitoring and episodes had resolved by the following morning. On review of the ECGs, and in liaison with an EP, the cardiology team considered various diagnoses including atrial fibrillation.
POCUS did not show any obvious structural heart disease, and formal TTE the following day was reported as normal.
After review by cardiology he was discharged home with EP follow-up.
Finally…
Remember that the lack of a delta wave on a resting ECG does not exclude an accessory pathway which could be causing AVRT. Two thirds of accessory pathways are concealed (no anterograde - i.e. atria to ventricle - conduction) on the baseline ECG.
and…
Always consider the additional “A to F” diagnoses below when reviewing the ECG of a young patient with pre/syncope or palpitations.
A is for: Arrythmogenic Right Ventricular Cardiomyopathy (ARVC)
B is for: Brugada Syndrome
C is for: Cardiomyopathy (HOCM)
D is for: “Delta Wave” of Wolff-Parkinson-White
E is for: “Extended QT” of Congenital Long QT syndrome
F is for: “Fright” i.e. Catecholaminergic Polymorphic Ventricular Tachycardia (CPVT)
alternatively…
Can, Quick, BRAD, Walk, Home
C is for: Conduction blocks
Q is for: QT long or short
B is for: Brugada
R is for: RV Infarction
A is for: Arrythmogenic Right Ventricular Cardiomyopathy (ARVC)
D is for: Dilated Cardiomyopathy (DCM)
Walk is for: WPW
Home if for: HOCM / LVH due to AS