Cardiology Case #6
Primary Author: Dr Alastair Robertson; Co-Authors: Dr Hywel James and David Law
Background:
BAT call at 5am:
68yo male, woke with central chest pain.
Noted to be bradycardic at scene.
RR 20, Sats 97% on air, HR 45, BP 132/89, temp 36.5.
Pre-hospital ECG reported as “Sinus Rhythm with 1st degree block, no ST changes.”
The patient arrives in ED and is stable.
He had had 100mcg IV fentanyl, and pain has improved to 5/10.
Here is his initial ECG
What is your interpretation?
Initial ECG
-
This is a crucial ECG to be able to recognise. Whilst not meeting STEMI criteria it is diagnostic of an Inferior Occlusion MI.
The rate is sinus bradycardia at 48/min, the PR is borderline prolonged at just over 200ms, the QRS is narrow (80ms) with normal axis.
There are hyperacute T waves in the inferior leads (II, III, aVF). These are broad based T waves which are large relative to the preceding QRS. In aVF you could fit the entire QRS complex into the T wave. These suggest acute myocardial infarction.
There is 0.5mm ST elevation in III, and perhaps in II as well. No ST elevation in aVF. This does not meet traditional STEMI criteria.
There are reciprocal changes, with subtle ST depression in leads aVL, I and V6.
This is diagnostic of inferior occlusion MI which requires urgent reperfusion.
Given the immediate concern for Inferior MI, POCUS was performed to assess for inferior regional wall motion abnormalities which would confirm the diagnosis.
In the meantime the patient was being loaded with aspirin and clopidogrel.
Cardiac POCUS
A single view is shown here. This is a parasternal short-axis view at the level of the LV mid-cavity.
-
View: parasternal short-axis.
Orientation and Assessment: intra-ventricular septum sits from about 8 to 12 o’clock with the RV behind this. Focus on the contraction, the area from 6 o'clock to 9 o’clock is not contracting as well as the rest of the myocardium which is contracting symmetrically inwards.
Interpretation: This shows subtle regional hypokinesis of the Inferior septum, and inferior free wall consistent with the suspicion of inferior ischaemia.
What to do now?
Here POCUS confirmed the initial suspicion of inferior occlusion MI which requires urgent reperfusion. As PCI was not available and there were no contraindications, the patient was thrombolysed with IV tenecteplase.
10 minutes later the patient was noted to be in a new cardiac rhythm.
What is your interpretation?
ECG 10 minutes post-thrombolysis
-
Broad complex rhythm with a rate of 85. Bizarre (NW) axis. No obvious p-waves before the QRS.
This is an Accelerated Idiopathic Ventricular Rhythm, which is a reperfusion arrhythmia. Such arrhythmias are common as myocardium is reperfused after thrombolysis.
There is a ventricular focus, and retrograde p-waves can be seen in lead V1 (just after the QRS), as well as in V5/6 (just on the J-point).
Reperfusion arrhythmias are often confused for ventricular tachycardia, but VT will have a rate of >120/min and there should be complete AV dissociation.
The patient remained stable and no treatment was necessary for the reperfusion arrhythmia. His ECG 1 hour post thrombolysis is shown below.
The hyper-acute T-waves in inferior leads has resolved, as has the ST elevation in II. T waves have flattened inferiorly, and there is some T wave inversion developing in III.
The reciprocal ST depression in I and aVL has resolved.
He remains bradycardic in a sinus rhythm with some PVCs.
He was haemodynamically stable and pain free so thrombolysis was deemed to have been successful.
POCUS Pearls:
Here the use of POCUS was useful in adding weight to the clinical suspicion of inferior MI that required reperfusion but did not meet STEMI criteria.
Basic POCUS:
Here a PSAX can be very useful in identifying regional wall motion abnormality. From a PLAX view, position the mitral valve in the centre of the screen and then rotate the probe 90 degrees clockwise (marker towards the patient’s left shoulder). Identify the mitral valve in cross-section (this looks like a fish-mouth) then fan distally down the LV.
The LV base will have the chordae visible as broken lines. The LV mid-cavity will have the papillary muscles visible as little blobs around 3- and 7-o’clock. The apex will be smaller, with the RV starting to disappear. You may need to move down a rib space, and come slightly more lateral to get the apical view.
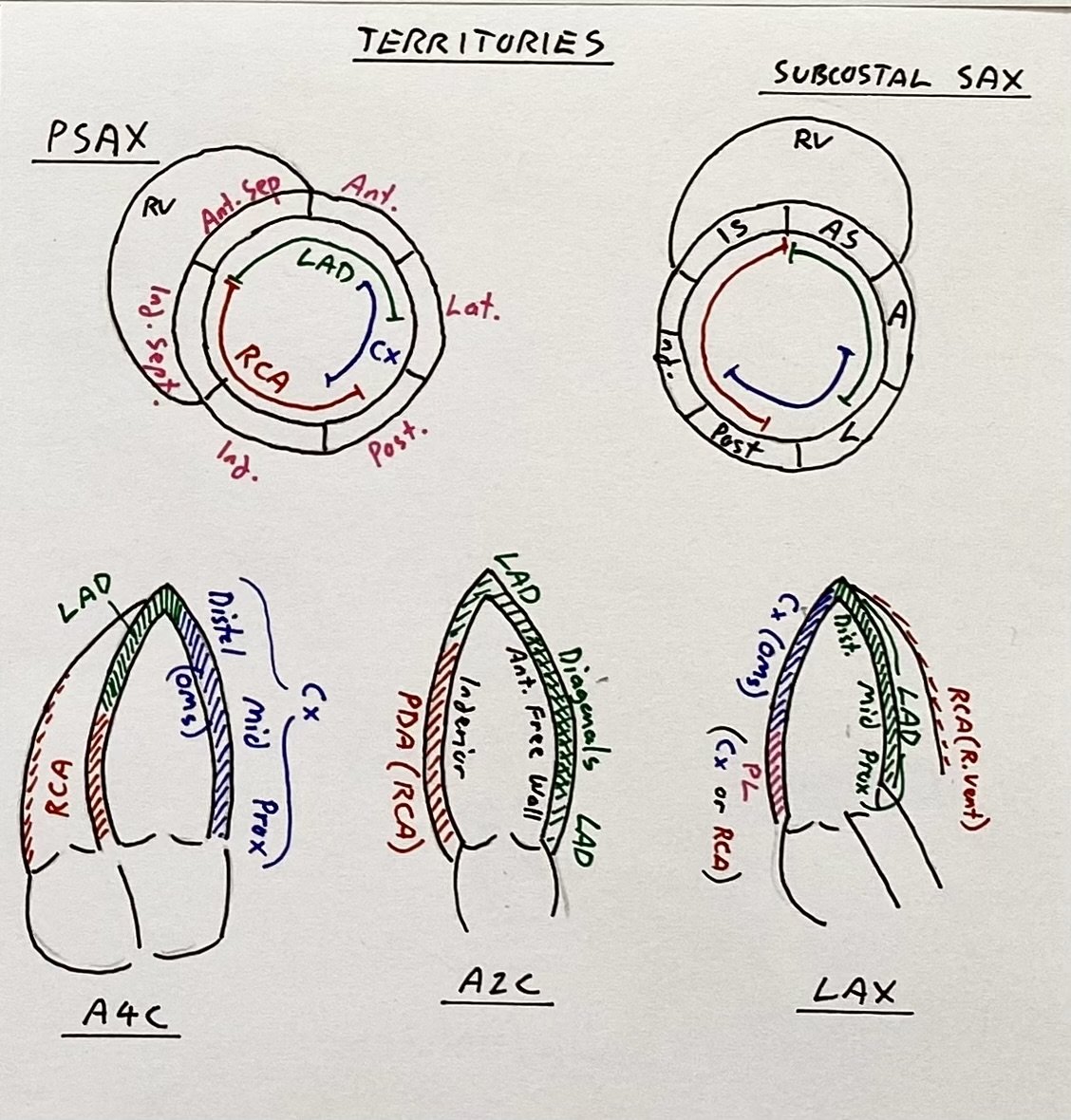
Familiarise yourself with the key vascular territories again to compare wth the apical view (see below).
Vascular territories on the key Apical, and Short-axis views.
Intermediate POCUS:
Apical views from the formal TTE are shown below (which was performed 48 hours later, and just prior to the patient proceeding for angiogram).
Here you can see an apical 4-chamber (top), apical 2-chamber (middle) and apical long axis (or 3-chamber - bottom).
The A4C shows hypokinesis at the apex, and extending into the mid-inferior septum.
The A2C shows the the proximal inferior wall, as well as the proximal anterior wall are working well, but there is hypokinesis towards the apex again.
The ALAX again shows hypokinesis wrapping around the apex.
This is interesting, as this suggests hypokinesis extending around the apex in the distal LAD territory whereas the inferior heart is usually supplied by either the RCA or the LCx. In RCA occlusion you would expect to the hypokinesis along the inferior wall in the A2C, and proximal septum on the A4C. In LCx occlusion you would expect to also see lateral wall hypokinesis.
Case Conclusion
Angiogram identified a ‘wraparound’ LAD which supplied the inferior aspect of the heart. There was a distal LAD lesion thought to be the culprit which was stented.
Initial troponin was 14, but the next troponin was 12,000.
The patient did well and was discharged home the day after his angiogram.
Focus on Inferior STEMI:
Inferior STEMI accounts for around 40% of MIs, with a 2-9% inpatient mortality. aVL is classically the reciprocal lead where you will see ST depression.
80% are due to right coronary occlusion
Look for ST elevation in III > II and reciprocal ST depression in I
Assess for signs of RV infarction (ST elevation in V1 and V4R)
18% are due to L circumflex occlusion
Look for ST elevation in II > III
Often no reciprocal change in lead I (or ST elevation if lateral involvement)
Lateral ST elevation (V5/6)
2% are due to a wraparound LAD such as this case here
Echo may show apical septal hypokinesis which extends into distal inferior territory rather than purely inferior hypokinesis.
Complications of Inferior STEMI
Be prepared to manage:
Bradyarrythmia (due to supply of the AV node by the RCA in 80% of people)
RV infarction (may require cautious fluid balance, may be preload dependent). GTN is not contraindicated in inferior MI but must be used very carefully.
Posterior infarction due to supply of the posterior wall by the RCA.
Here an RV focussed view is obtained by hooking laterally from the apical 4-chamber view. This shows the true RV size, whilst apical, or more medial windows often cut the RV obliquely, giving an artificial impression of a dilated RV.
Reassuringly the RV appears to have good function and is not dilated.
Finally…
Learn to recognise hyper-acute T waves. If you are interested in learning more you may find the link below interesting.